Female health and care staff report deteriorating health because of COVID-19: The physical and mental wellbeing of female health and care staff in England significantly worsened as a result of working through the COVID-19 pandemic with a marked deterioration since last summer, the results of a new survey show.
The poll, carried out by the NHS Confederation’s Health and Care Women Leaders Network in February and March in the aftermath of the deadly peak of the virus in January, shows a significant rise in women working across health and care reporting a negative impact from their work on their mental and physical health, as a result of the pandemic.
More than 80 per cent of female respondents who completed the new survey – including nurses, doctors, managers, admin staff, and allied health professionals – reported their job had a greater negative impact than usual on their emotional wellbeing as a result of the pandemic, up from 72 per cent last summer. The results also showed 65 per cent reported a negative impact on their physical health – a 13-percentage-point jump from the last survey.
More than 1,200 NHS staff responded to at least part of the survey, carried out by the NHS Confederation’s Health and Care Women Leaders Network, with about 900 completing it in full, including more than 800 staff who identified as female. The results cover the responses of the women who answered every question.
The survey, which follows a similar poll carried out in June, does highlight some of the positive experiences of female staff during the COVID-19 crisis, including increased opportunities for flexible working, improved teamwork and better access to technology, and some of the hopes of staff for the future, including continued flexible working and better work/life balance.
But the most recent findings also show how significantly caring responsibilities outside work have grown since the summer for female staff. The results showed women working in health and care took on an average of about 13 hours extra a week in unpaid caring responsibilities, compared with before the pandemic, rising from about 11 hours extra a week in the last survey. There was also an increase in the total number of hours spent each week on these responsibilities compared with the summer, from an average of about 18 to about 20.
In particular, respondents with children reported being far more involved in these tasks than usual. This is likely linked to the prolonged closure of schools, and reduced working hours. This has serious implications for career progression opportunities, the survey results suggest.
Furthermore, female health and care staff with long-term health conditions reported a greater negative impact of the pandemic on their physical health compared with those without long-term conditions, and they also reported feeling less safe sharing concerns with managers. Perhaps most startlingly, nearly 87 per cent of respondents with long-term conditions reported that their job has had a more negative impact on their emotional wellbeing since the pandemic started, compared with 78.9 per cent of those without.
The Network will work with employers and national partners to understand the reasons for this disparity, and what more needs to be done to support the workforce in light of these findings.
The findings also give weight to calls made by the NHS Confederation for extra investment to support the workforce in the long-term, and head off a haemorrhaging of doctors, nurses and other frontline health workers, in a letter to the Prime Minister jointly signed by NHS Providers, the British Medical Association, the Royal College of Nursing, the Academy of Royal Medical Colleges and Unison.
Samantha Allen, chair of the NHS Confederation’s Health and Care Women Leaders Network and chief executive of Sussex Partnership NHS Foundation Trust, said: “These survey findings underline the importance of the focus being placed upon the physical and mental health of NHS and care staff. As the majority of the health and care workforce is female, a significant burden in overcoming the enormous challenges we face in recovering services will fall on the shoulders of women.
“We need to see tailored support specifically for the needs of female staff and this should include recruitment, retention, flexible working and career progression. We are concerned that if these issues are not addressed, it could intensify the impact on our workforce at a time when the NHS can ill-afford to lose any more staff. We are worried the impact of COVID-19 could set the NHS back further when we want to create the conditions where our workforce is valued and all can progress in their careers, particularly those who work less than full time.
“We need to make sure we look after people, after the incredibly difficult experiences they have been through during the pandemic while supporting patients, families and carers and with the increased responsibilities of caring for children and adults outside of work. Looking after our staff will enable us to continue looking after the people who need our services. The findings of this survey must be a driver of real and lasting change.”
Rebecca Smith, managing director of NHS Employers, which is part of the NHS Confederation, said: “These findings again highlight the burdens faced by the female health and care workforce as a result of working through the COVID-19 crisis. Much of the responsibility for caring outside work falls to women, and for NHS staff, this is alongside the additional pressures they have faced working through the most challenging year most of them will have ever experienced. We now need additional investment from Government, coupled with the existing and ongoing direct support by health and care organisations, to make sure the female workforce is properly looked after. As we come out of this crisis we must continue to do all we can to protect and support our staff.
“The results of the survey also provide some valuable insight into the positives that have come out of the pandemic, such as increased opportunities for flexible working and improved teamwork. NHS Employers will continue to work with NHS organisations to make sure these positives are maintained beyond the crisis, and embedded into new and innovative ways of working. We will also continue to provide guidance on support for the female workforce.”
Dr Henrietta Hughes, National Guardian for the NHS, said: “The pandemic has impacted on us all, emotionally and physically, and has exacerbated inequalities, which can no longer be tolerated. This report shows how vital it is, not just for people to feel able to speak up about anything which gets in the way of them doing their job, but for managers to be supported to listen up and for leaders to follow up so that the right actions are taken.”
Kate Jarman, director of corporate affairs at Milton Keynes University Hospital and co-founder of FlexNHS, said: “The impact of COVID-19 on women and on the emotional and physical health of women cannot be underestimated. There is a real and present danger of setting gender equality back, particularly for women in the paid labour market, and in failing to recognise and act on the extraordinary burden of unpaid domestic labour and care that is carried, predominantly, by women.
“The vast majority of the health and care workforce are women – we have a critical role in tackling the equality gap that the pandemic has widened.”
- Combination of drugs could prevent thousands of heart attacks - 21st April 2025
- UQ Study Links Poor Teen Diets to Heavy Social Media Use - 21st April 2025
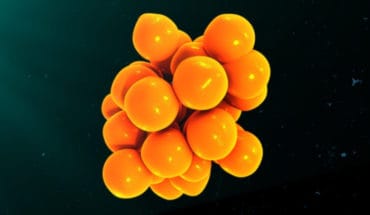
- Gut microbiome could delay onset of type 1 diabetes - 3rd April 2025