Don’t overlook fertility problems in your man, says Dr Catherine Hood, a consultant in psychosexual medicine, health writer and broadcaster. ‘Women are often quick to blame themselves if they don’t get pregnant, and overlook the fact that it is increasingly likely that the problem lies with their partner.’
The number of men diagnosed with severe infertility has doubled in a decade and studies confirm that sperm counts are in steady decline, falling by 1.4 per cent every year — a 52.4 per cent drop between 1973 and 2011.
As many as one in seven couples has difficulty conceiving and male issues, primarily poor semen quality, are now the sole cause, or a contributing factor, in 50 per cent of cases.
As many as one in seven couples has difficulty conceiving and male issues, primarily poor semen quality, are now the sole cause, or a contributing factor, in 50 per cent of cases.
But fewer than five per cent of UK fertility clinics hold accreditation confirming they comply with World Health Organisation guidelines on semen analysis. ‘In my opinion, too many couples are considering in-vitro fertilisation before exploring simpler, and far less expensive therapies, which address poor sperm counts or motility.’
‘In research which I presented at the London Fertility Show held this weekend, I called for an urgent review of treatment guidelines to address this rise in male infertility and alert couples to the efficacy of low-cost alternatives to female-focused IVF.
I believe some couples could save thousands of pounds by exploring less invasive infertility treatments such as intracervical insemination (ICI) — the use of a cervical cap to hold sperm close to the cervix — and intrauterine insemination (IUI), before resorting to IVF.’
In clinical trials, ICI has a success rate of around 20 per cent and can be performed in a home setting, which is far less stressful than attending a hospital or fertility clinic. This is important because we know that women who are stressed are less likely to conceive.’
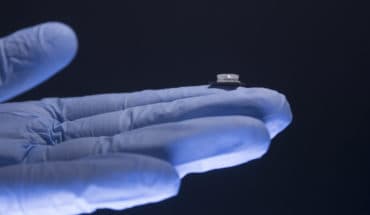
Research for The Stork, a clinically proven home-use ICI device, found that only nine per cent of couples who were having trouble conceiving were aware of these DIY conception aids.
By contrast, 57 per cent of women struggling to start a family said they would consider IVF, even though 61 per cent admitted they were worried about the cost.
Current guidance from the National Institute for Health and Care Excellence (NICE) overlooks ICI, and advises against IUI, in favour of IVF — which costs around £5,000 and has a success rate of only two to 33 per cent, depending on the woman’s age.
It also says the NHS should offer up to three cycles of IVF to women under 40 who have not conceived after two years of trying for a baby — advice which is flouted by 87 per cent of the Clinical Commissioning Groups which provide health services.
NHS rationing means that 60 per cent of IVF treatment is privately funded, and with 50,000 women seeking treatment every year, fertility treatment has become a very big business. There is not enough awareness of cheaper and successful alternative treatments. It makes sense to try these first.
A single cycle of IVF costs around £5,000 and some clinics recommend additional tests and therapies which can push the cost much higher. By comparison, IUI costs around £1,000 and The Stork home-use ICI device costs £99.99.
Says Dr Hood: ‘For many couples, it makes sense to try a low-cost option, such as The Stork, first. It is a relatively inexpensive conception aid which works in the same way as ICI, a clinically proven treatment with a success rate of 20 per cent.’
- Don’t overlook fertility problems in your man - 6th November 2017