Novel computational methods provide new insight into daytime alertness in people with sleep apnoea.
New polysomnography parameters are better than conventional ones at describing how the severity of oxygen desaturation during sleep affects daytime alertness in patients with obstructive sleep apnoea, according to a new study published in European Respiratory Journal.
Inadequate sleep is widely recognised as a significant public health burden in Western countries. Good quality sleep is also crucial for maintaining neurocognitive performance. An increasing number of occupational accidents and absences, as well as traffic accidents, are caused by factors decreasing sleep quality.
Obstructive sleep apnoea (OSA) is one of the most prevalent sleep disorders, affecting more than 20% of the adult population in Western countries. OSA is attributed to daytime symptoms of shortened daytime sleep latencies as well as chronic fatigue and sleepiness. Furthermore, OSA is related to poor neurocognitive performance and inability to sustain attention.
Neurocognitive disorders cover the domains of learning and memory, language, executive functioning and complex attention, among others. One test assessing neurocognitive performance is the psychomotor vigilance task (PVT), which evaluates the domain of complex attention by measuring repeated responses to visual stimuli, thus assessing a person’s ability to sustain attention.
The researchers investigated the role of conventional and novel polysomnography parameters in predicting PVT performance in a sample of 743 OSA patients. The patients completed the PVT test in the evening before undergoing a polysomnography.
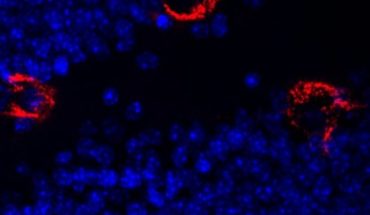
All polysomnography recordings were scored manually by experienced sleep technicians who regularly participate in scoring concordance activities. All apnoeas, hypopnoeas and desaturations were scored manually in accordance with established guidelines.
The researchers found that their novel parameters describing the severity of intermittent hypoxaemia, i.e. oxygen desaturation during sleep, are significantly associated with an increased risk of impaired PVT performance, whereas conventional OSA severity and sleep fragmentation metrics are not. This finding is also supported by the group’s previous study showing that OSA-related objective daytime sleepiness is more strongly associated with the severity of individual desaturations than the number of apnoeas and hypopnoeas.
According to the researchers, parameters quantifying desaturations based on their characteristic properties have a significant association with impaired vigilance and ability to sustain attention. Furthermore, an increase in the apnoea–hypopnoea index or the oxygen desaturation index does not significantly elevate the odds of having impaired PVT performance.
“Our results highlight the importance of developing methods for a more detailed assessment of OSA severity and comprehensive analysis of PSGs. This would enhance the assessment of OSA severity and improve the estimation of risk and severity of related daytime symptoms,” Early Stage Researcher and first author Samu Kainulainen from the University of Eastern Finland concludes.
Read the full report at European Respiratory Journal 2020 55: 1901849; DOI: 10.1183/13993003.01849-2019
Photo credit : Shutterstock / By fizkes
- KFSH featured in Nature Genetics - 13th February 2026
- Marking 150 years since Public Health Act 1875 - 13th February 2026
- Colorectal cancer rate rising amongst the young - 13th February 2026