A pioneering programme which is bringing affordable, reliable and portable diagnostics for multiple diseases to sub-Saharan Africa is set to be presented at an event linked to the United Nations General Assembly this week.
On Thursday 14 September, members of the Digital Innovations and Diagnostics for Infectious Diseases in Africa project, or DIDIDA, will be part of an event organised by the International Science Summit around the 78th United Nations General Assembly (UNGA78).
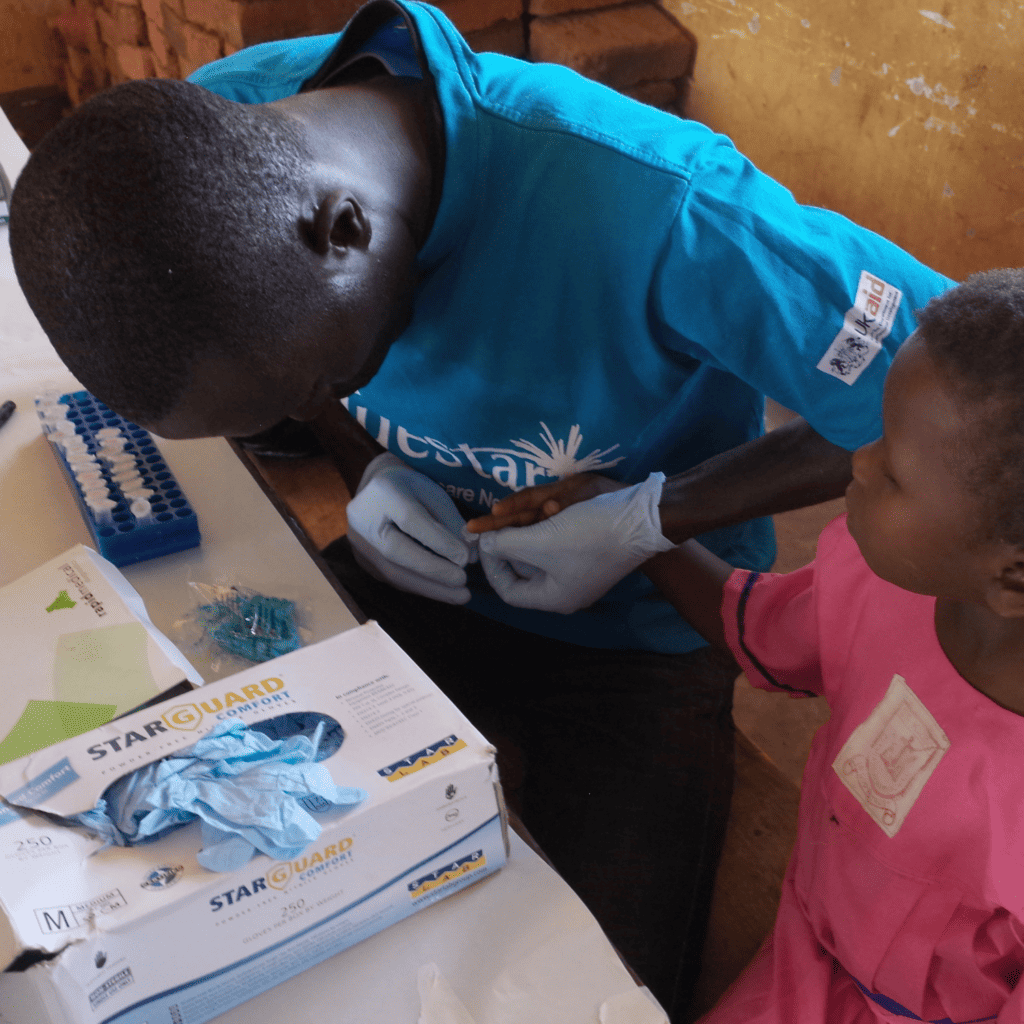
DIDIDA, supported by £6.75m in funding from the European Union and UKRI, is developing new ways to use lateral flow tests, similar to those used to diagnose COVID-19, to diagnose more than one disease at the same time in even the most remote locations.
The technology aims to diagnose multiple infectious conditions including the five leading causes of death in sub-Saharan Africa: severe respiratory infections, HIV/AIDS, diarrhoea, malaria, and tuberculosis. Together, they kill more than six million people each year.
The tests are run on portable devices which use a process called loop-mediated isothermal amplification to test DNA samples collected on lateral flow strips with remarkable sensitivity.
The tests amplify the nucleic acids in patient samples to identify the genetic material of infectious agents. They are sensitive enough to identify infections even when patients show no outward symptoms.
Those devices are linked to mobile phones, where an app developed by the team uses artificial intelligence to analyse the test results and provide a diagnosis. Health workers will be able to deliver recommendations for treatment directly to patients.
The results can also be shared directly from the app with regional or national healthcare authorities to help create a real-time dashboard of infections of diseases, including asymptomatic conditions – a key consideration for strategies which aim to eliminate disease outbreaks. The dashboards will also help clinicians to explore the links between infectious and non-communicable diseases including cardiovascular disease and diabetes.
The dashboard will also help authorities monitor the spread of diseases as climate change-driven changes in temperature drive parasite-carrying insects beyond their usual home territories.
DIDIDA’s funding also supports the creation of a new graduate school in sub-Saharan Africa. The school will train 18 new PhDs in areas including artificial intelligence, manufacturing, engineering and synthetic biology to help them make further improvements to the diagnostic technology. They will also train health workers in how to administer the tests.
Professor Jon Cooper, of the University of Glasgow’s James Watt School of Engineering, is DIDIDA’s principal investigator. DIDIDA brings together 14 partners from eight countries: Kenya, Senegal, Tanzania, Uganda, the United Kingdom, France, the Netherlands, and Italy.
The project builds on previous work undertaken by Prof Cooper and his Glasgow colleague Prof Julien Reboud, which prototyped and tested the diagnostic techniques to monitor conditions including malaria and schistosomiasis in Uganda, with both now delivering aspects of DIDIDA with partners in Africa.
Professor Cooper said: “I’m pleased to have this opportunity to showcase DIDIDA, which aligns with many of the United Nations’ sustainable development goals, including Good Health and Wellbeing, Quality Education and Climate Action.
“More than 50% of the population of sub-Saharan Africa lacks access to essential health services, and in rural areas it’s often difficult for patients to get an accurate diagnosis. DIDIDA is working to tackle that problem by providing a system that can be used anywhere to provide patients with appropriate diagnosis and the correct treatments. That will help improve patient outcomes and reduce the antimicrobial resistance that can come from offering patients ineffective drugs based on incorrect diagnoses.
“Just as importantly, the results collected and securely shared with regional and national health authorities will help them make better-informed decisions about disease management and treatment.
“By the time the project is complete in 2027, we’ll have trained a new generation of African experts in cutting-edge diagnostic techniques which have the potential to radically transform the way public health is tested, treated and monitored.”
Dr Harriet Mpairwe, from the Uganda Virus Research Institute, and Emmanuel Milimo, of Pharmaccess Kenya, are partners on the DIDIDA project and will present their work to the General Assembly alongside Prof Cooper.
Dr Mpairwe said: “One of the aims of DIDIDA is to explore better diagnostics for patients presenting with fever. Individuals often present to doctors with febrile illness which could be caused by a number of different infectious diseases, including malaria. Ensuring that the correct treatment is given will have clear benefits not just to the induvial but the whole community”
Mr Milimo added: “Pharmaccess is very pleased to be part of this exciting project. We are an international non-profit organization with a digital agenda dedicated to connecting more people in sub-Saharan Africa to better healthcare. Our platforms can not only be used to look at changes in infectious disease prevalence across communities but also, in the future can be linked with meteorological data to explore how climate changes might influence the spread of disease.”
The University of Glasgow’s contribution to DIDIDA brings together bionegineers and medics at the University’s Mazumdar-Shaw Advanced Research Centre (ARC). The ARC is specifically designed to encourage the kind of cross-disciplinary working that characterises DIDIDA.
The event which will showcase the DIDIDA team’s work, which is titled ‘Transformative digital diagnostic technologies with Imperial College London’, will be held online between 9am and 11am on Thursday September 14.
Experts from academia, industry and health agenciesfrom the UK and Africa will present their insights into developing and testing transformative digital diagnostics technologies in Africa, and their contributions to achieving UN sustainable development goals.
For more information on the event, or to sign up to attend online, visit
- RV3-BB rotavirus vaccine at birth boosts microbiome - 8th May 2025
- No Mind Left Behind: Support the Carers - 4th May 2025
- Climate change causes longer pollen seasons in capital cities - 4th May 2025