How a virus transforms immune cells into leukaemia uncovered by researchers: An international team have mapped how the HTLV-1 virus causes a rare leukaemia in some people, providing clues on how to stop it happening.
The team, led by Imperial College London and Kumamoto University in Japan, used single-cell analysis to show how the virus over-activates T-cells, key immune cells in our blood, causing them to turn cancerous.
Our work highlights a key mechanism for this change and provides us with new directions to search for ways to interfere with the process, potentially preventing the cancer from developing.Dr Masahiro Ono
The rare cancer, called adult T-cell leukaemia/lymphoma (ATL), develops in around five per cent of people infected with the HTLV-1 virus, but only several decades after initial infection. HTLV-1 infects T-cells specifically and transforms them into leukaemia cells, but the time lag has made it extremely difficult to determine how this transformation occurs.
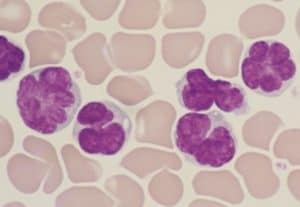
Virus-induced leukaemia cells. Credit: Dr Utsunomiya
ATL can progress slowly or aggressively, but there is no standard treatment for high-grade ATL, and the condition has a high relapse rate after treatment with chemotherapy and antiviral drugs.
The team’s results, published today in The Journal of Clinical Investigation, reveal that the virus hijacks the activation machinery of T-cells, causing them to persist at a high level of activation, gradually becoming malignant.
Great need to understand the virus
Co-lead researcher Professor Yorifumi Satou, from Kumamoto University is a virologist studying HTLV-1. He said: “While only a small percentage of people with HTLV-1 viral infections go on to develop adult T-cell leukaemia/lymphoma, there are estimated to be around five to ten million carriers of the virus worldwide, and in some areas it is endemic – for example there are around one million cases in Japan.”
Co-lead researcher Dr Masahiro Ono, from the Department of Life Sciences at Imperial, is an immunologist and cell biologist who brought his knowledge of T-cells to the project. He said: “There is therefore a great need to understand how the virus turns our T-cells against us in the progression to cancer. Our work highlights a key mechanism for this change and provides us with new directions to search for ways to interfere with the process, potentially preventing the cancer from developing.”
Leukaemias are cancers originating from blood or bone marrow cells, characterised by large increases in the number of abnormal white blood cells. T-cells are special kinds of white blood cells that are crucial for fighting off invaders, such as viruses and bacteria.
The HTLV-1 virus inserts itself into one type of T-cell, and, to begin with, remains there in a ‘latent’ state, not releasing any new virus particles or causing any ill effects. For many such carriers of the virus, this never changes, but in around five per cent of carriers, after decades of latency the virus reawakens and affects the T-cells’ functioning.
Over-reactive T-cells
The team studied more than 87,000 T-cells from virus-free donors, healthy carriers of the virus, and patients with ATL. They sequenced the RNA (a simpler form of DNA) from these cells to find out how the virus and the T-cells were interacting.
They revealed that, in people who progressed to ATL, HTLV-1 made infected T-cells highly activated and over-reactive, causing them to over-produce proteins that keep them proliferating and helping them avoid other parts of the immune system that would usually remove rogue cells.
The team thinks that these changes made the overactive T-cells more vulnerable to DNA damage, such as through chemical agents or radiation, accelerating their transition to a cancerous state.
Further study of the processes involved, say the authors, will lay the foundations for potential new treatment options. Dr Ono said: “For example, the chronic activation of T-cells could be halted by molecules that block signalling pathways that tell the cells to activate. Alternatively, treatments could target the proteins the activated T-cells create to help them proliferate.”
The study was performed by the collaborative team led by Professor Yorifumi Satou from Kumamoto University, Japan and Dr Masahiro Ono from Imperial. The collaborative research groups include the University of Tokyo, Saga University, and Kagoshima University, and clinical collaborations include hospitals in Kyushu island.
–
‘HTLV-1 infection promotes excessive T cell activation and transformation into adult T cell leukemia/ lymphoma’ by Benjy J.Y. Tan et al. is published in The Journal of Clinical Investigation.
- Gut microbiome could delay onset of type 1 diabetes - 3rd April 2025
- The da Vinci 5 Robot Is Set To Transform Bariatric Care: - 31st March 2025
- Beyond money: the hidden drivers fuelling child food insecurity - 31st March 2025